Abstract
Introduction
When added to cytarabine (Ara-c) or hypomethylating agents (HMA), the BCL2 inhibitor, venetoclax (VTX), has been reported to improve response and overall survival (OS) rates. However, resistance and relapse still occur in the majority, and, although alterations in MCL1 and BCLXL are noted at relapse, identification of prognostic features remain unknown, notably not correlating with expression of the BCL2 target. Identification of prognostic markers could guide VTX use in patients and/or post-remission therapy. We searched for protein expression targets individually and collectively to predict VTX response and relapse in AML.
Methods
Reverse Phase Protein Array (RPPA) was performed on diagnostic leukemia samples of 818 adults with AML, of which 143 received VTX including 33 in combination with high dose Ara-C, 5 with standard dose Ara-C, 50 with HMA, and 13 with HMA and targeted therapy. Protein expression levels were evaluated using 390 validated antibodies were analyzed in the context of clinical data compiled by retrospective chart review. Pearson correlation was used to identify significant protein-protein correlations. Survival curves were generated by the Kaplan-Meier method and survival data was analyzed by multivariate cox regression model. Protein expression signatures were identified by hierarchical clustering and predictive models of classifiers were determined by classification and regression trees (CART) analysis.
Results
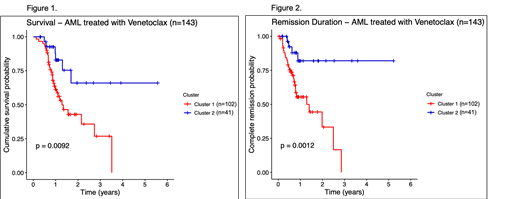
We queried the 390 proteins assayed in the 143 VTX treated patients to identify proteins individually prognostic (p<0.01) for OS (n=27) or remission duration (RD, n=44). Notably, neither MCL1, BCLXL nor BCL2 expression at diagnosis were prognostic of OS or RD. From these, unbiased hierarchical clustering revealed two cohorts (N=102 & 41 patients) for OS and RD. The clusters were similar for clinical features with no significant differences noted for, age, gender, performance status, cytogenetics, or the presence of molecular mutation markers FLT3.ITD, IDH1/2, NPM1 or TP53. The groups did not differ by therapy combination. Remission rates were insignificantly less in cluster 1 (61% vs 77%). Clear differences were observed for OS with estimated 3-yr overall survival 27% vs 66% (p=0.009, Figure 1) and relapse risk (RR) at 1-yr 45% vs 18% (p=0.001, Figure 2) in cluster 1 vs 2, respectively. In multivariate analysis, protein cluster membership was in independent prognostic factor for OS (along with TP53 and NPM1 mutations) but unfavorable cytogenetics was not. Prognostication did not vary based on cytogenetics or therapy received. For RD, protein cluster membership and unfavorable cytogenetics were the only independent predictors. Of the 44 proteins in the protein signature, CART modeling identified 3 - SPI1, NOTCH1.cle, and PTPN12 - that could predict clustering with a computed accuracy of 94.3%. Similarly, when these three proteins were used as training variables for random forest classification, the error rate was 3.7%. Several previously unrecognized potential therapeutic targets for preventing VTX resistance were also identified.
Discussion
Protein expression patterns, individually and in combination, were very highly predictive of outcome to VTX containing combination chemotherapy. A group with lower response rates, higher relapse rates, shorter RD and inferior OS was defined. A kit to prospectively determine cluster membership is in development. If validated this could be used to triage high-risk patients to alternate therapies, such as transplant, in CR1. Many new targets for combination therapy to prevent VTX resistance were identified and need to be tested in the laboratory for clinical relevance.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal